Update 2022-2023
Greetings and welcome to the second update from The Permanente Medical Group’s Delivery Science and Applied Research (DARE) program!
TPMG’s DARE program provides infrastructure, connections, and analytic support to clinician-researchers who are answering questions that will change care within Kaiser Permanente.
Started in 2018 under the leadership of TPMG’s Chief Executive Officer and Associate Executive Directors, it is a collaboration between clinician investigators and Division of Research scientific experts, to inform large numbers of rapid-cycle, evidence-based innovations.
The DARE program includes:
- A DARE support team to consult on ideas to facilitate successful clinician-led research;
- A one-stop idea/funding support submission process to provide consistent, rapid, centralized project idea review and support for three DARE project funding mechanisms;
- The TPMG Physician Researcher Program, which provides high-level support to selected clinician investigators to conduct clinically relevant research;
- Specialty-specific research networks that build communities of evidence-driven clinicians.
- Centrally available tools, training, connections, and collaborations to speed the process from research results to implementation;
- Expanded financial support for disseminating results in publications and national meetings.
In the following pages, we invite you to explore these resources and the “DARE Dozen”: twelve sample DARE supported projects drawn from approximately 120 investigations underway across different specialties in 2021–2023 alone. These projects are poised to change care or have already done so; we hope you enjoy reading about these and invite you to learn more about others included here and at kp.org/dare.
We look forward, in 2024-2025, to further supporting TPMG’s ongoing strategic areas of focus. It has been an active and exciting last two ears — the incredible talent and productivity of TPMG’s clinician-investigators and their dedication to evaluating and improving care is inspiring. We look forward to supporting your ideas, and always welcome new recommendations to improve.
Warm regards on behalf of the entire DARE team,
Douglas Corley, MD, PhD
Director, Delivery Science and Applied Research, TPMG
Tracy Lieu, MD, MPH
Director, Kaiser Permanente Division of Research
Yi Fen Irene Chen, MD and Smita Rouillard, MD
Associate Executive Directors, TPMG
Featured Projects - "DARE Dozen"
Delivery Science Grants Program
| Authors | Assiamira Ferrara, MD, PhD, Mara Greenberg, MD |
|---|---|
| Challenges | Prenatal care visits are extremely common and direct important screening tests for pregnancy-related hypertension and diabetes. Telehealth may be a useful approach for these routine visits, but its impact on birth outcomes is unknown. |
| Existing Evidence | Pregnant patients and their providers perceive the use of telemedicine as a positive experience, though its effectiveness for prenatal care outcomes is unknown, including its potential role for decreasing differences in accessing care by location, demographics, and socioeconomic status. |
| Target Population | Individuals pregnant during and before the COVID-19 pandemic |
| Intervention or Exposure | Visit type: office only, partial telehealth, full telehealth (pre-pandemic vs. increased telehealth during pandemic); and COVID infection from 30 days before conception to 7 days after delivery |
| Outcomes/Key Findings | A hybrid model of prenatal care using a combination of in-office and telemedicine visits is effective and could be used beyond the pandemic period. A higher (25%) proportion of prenatal visits from telemedicine intra-pandemic vs. 14% pre-pandemic provided similar comparable detection rates of gestational diabetes, preeclampsia, preterm birth and NICU admission rates; no differences were seen between people of different race, ethnicity, or measures of neighborhood deprivation. Pregnant individuals with SARS-CoV-2 infection had higher risk of severe maternal morbidity (HR 2.45, 95% CI:1.91, 3.14), preterm birth (<37 weeks; 2.07 [1.75, 2.46]) and venous thromboembolism (3.08 [1.09, 8.74]). |
| Resulting Action/Change | These data support a next-step KPNC pilot of a nationally designed hybrid prenatal care model for low risk pregnancies. |
| Additional Recommendations | Evaluating other pandemic-associated prenatal care changes, including decreased early-pregnancy screening for gestational diabetes and change from multimodal aneuploidy screening to cell-free DNA screening to inform their inform continuation of these novel care patterns. |
| Implementation Tools | Telemedicine contact, device, and screening protocols for prenatal care. |
| Implementation and Follow-up Measures |
Proportions of pregnancies using telemedicine or hybrid approaches; completion of recommended screenings; detection rates of gestational diabetes, pre-eclampsia, and diagnosed depression; differences by demographics and medical center. |
| Reference | 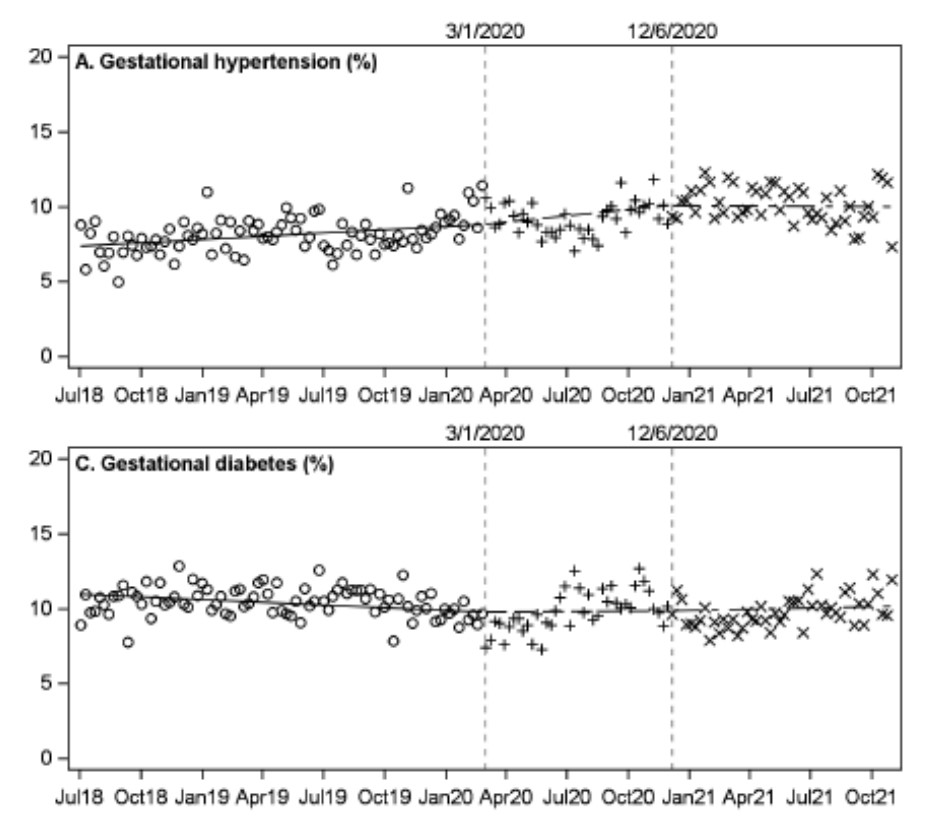 https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2807379 https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2807379 |
| Authors | Lisa J. Herrinton, PhD; Keras Lo, PharmD; Mubarika Alavi, MS; Stacey E. Alexeeff, PhD; Kerri M. Butler, PharmD; Carter Chang, MD; Christopher C. Chang, PharmD; Virginia L. Chu, PharmD; Ashok Krishnaswami, MD, MAS; Lynn H. Deguzman, PharmD; Stephanie Prausnitz, MS; Maisha Draves, MD, MPH; Michael D. Mason, MD |
|---|---|
| Challenges | Many older patients use large numbers of medications, which may increase the risk of adverse events without benefit. A proposed deprescribing intervention with pharmacists may help; however, its effectiveness is unknown, it is resource intensive, and it may create unanticipated adverse events from stopping medications. |
| Existing Evidence | Deprescribing has been implemented in numerous settings, including currently with Kaiser Permanente, but typically it involves only single drug classes. Using multiple single drug deprescribing efforts is inefficient, but little data exist on the potential beneficial or harmful impacts of “bundled” multi-drug deprescribing strategies. |
| Target Population | KPNC members aged ≥76 years using ≥10 prescription drugs, excluding those with a history of transplant; dialysis; hospice care; or a cancer diagnosis, oncology visits, or cancer treatment within a year. |
| Intervention or Exposure | A randomized trial of bundled multi-drug deprescribing using integrated pharmacist review of >20 drug classes within a single workflow, developed with relevant medical specialists, and using random patient assignment. |
| Outcomes/Key Findings |
A large pragmatic clinical trial of pharmacist-directed multi-medication evaluation and patient counseling/deprescribingresulted in:
|
| Resulting Action/Change | Informed value-based care to not proceed with a planned large, complex intervention that would have required >10 pharmacist equivalent positions and complex coordination between pharmacy and adult & family medicine for full implementation. |
| Additional Recommendations | Pragmatic trials prior to full implementation are feasible and have clear benefit in understanding effectiveness and to evaluate for potential unanticipated harms. |
| Implementation Tools | Drug protocols, medication discontinuation/continuation guidelines for disease-specific essential conditions, monitoring protocols/variables for adverse effects |
| Implementation and Follow-up Measures |
Drug protocols, medication discontinuation/continuation guidelines for disease-specific essential conditions, monitoring protocols/variables for adverse effects |
| Reference | 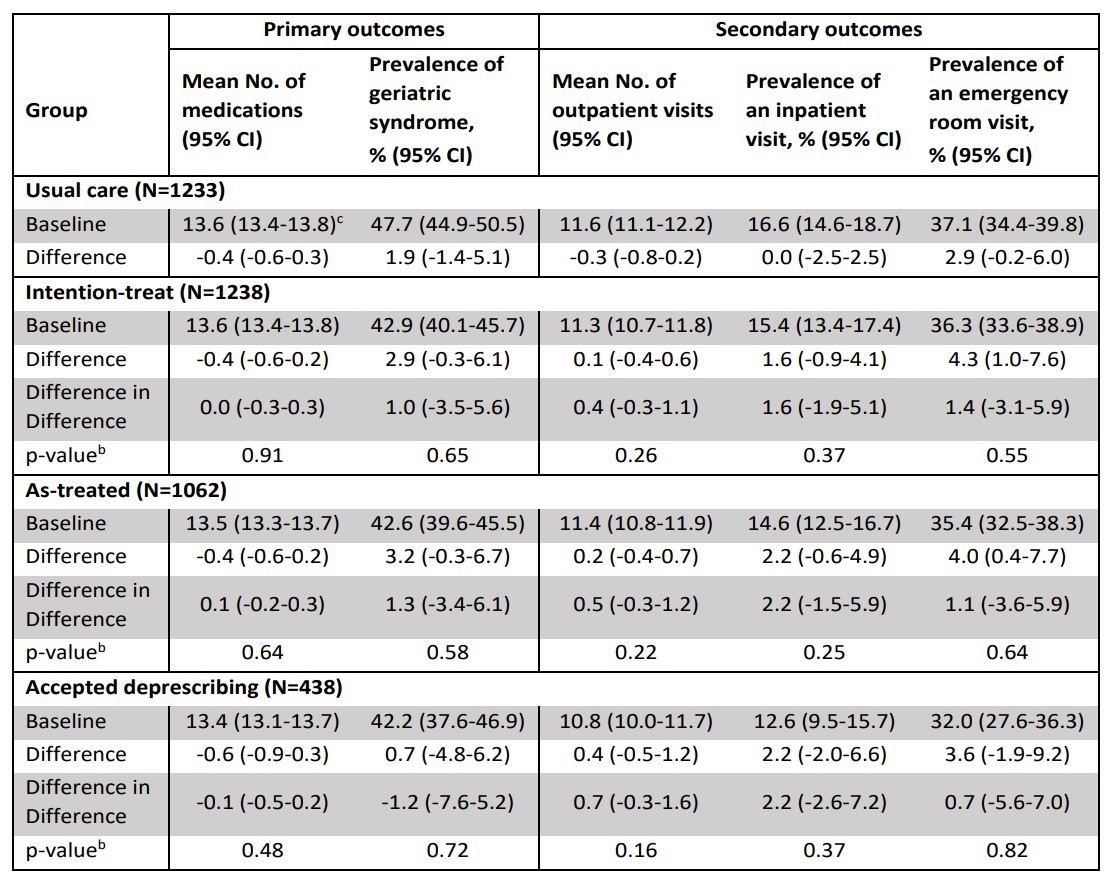 https://pubmed.ncbi.nlm.nih.gov/37428504/ |
| Authors | Adrian Hinman, MD, David Lee, M.D., Kamran Sadr, M.D., Kasey Cortese, M.D., Catherine Lee, Ph.D., Stephanie Prausnitz, M.S.., Andrew Avins, M.D., M.P.H. |
|---|---|
| Challenges | Adductor canal catheters are a common, invasive, and potentially beneficial method for improving post-operative pain control among patients undergoing total knee arthroplasty, but it is unknown if their use provides benefits beyond simpler pain management techniques, such as intra-operative peri-articular injection. |
| Existing Evidence | In the last 7 years, the length of stay for total knee replacement patients in KPNC decreased from 3 days to <1 day, partially from improved pain control. Pilot KPNC data, and external trial data suggest adductor canal catheters may not substantially influence length of stay, opioid use, or pain scores beyond peri-articular injection. They are also associated with complications (e.g. leaking, dislodging, bleeding, hematoma, prolonged neuropraxia), that can require additional outpatient & ED visits, and substantial resources. |
| Target Population | All patients undergoing a non-complex unilateral total knee replacement who are eligible to receive an adductor canal catheter |
| Intervention or Exposure | Use of an adductor canal catheter as a supplement to other ERAS pain control protocols |
| Outcomes/Key Findings | Pain control and postoperative use of opioid medications were comparable (non-inferior) between patients using vs. not using adductor canal catheters as a supplement to other pain management strategies after knee replacement surgery. Complex and invasive multi-modal pain treatments using adductor canal catheters may not provide additional benefit for pain control, not impact length of stay, and increased costs/effort beyond simpler current methods for pain management |
| Resulting Action/Change | The orthopedic and pain control services are evaluating whether to modify the current common use of adductor canal catheters in patients undergoing knee replacement. This would be projected, for similar outcomes, to result in: comparable pain control; fewer catheter-related complications; decreased operating room staff, anesthesiologist, & room time for insertion; decreased nursing time for patient education; fewer post-operative visits for complications and removal; and directly reduced catheter costs of $1.5 million annually for KPNC. |
| Additional Recommendations | For additional conditions, comparative evaluations of whether invasive multi-modality pain interventions may provide value beyond simpler interventions |
| Implementation Tools | Data summaries regarding comparable outcomes for patient & physician education |
| Implementation and Follow-up Measures |
Adductor canal catheter use, variation by medical center, physician, and patient demographics; post-discharge healthcare utilization (e.g. ED, office, phone visits) |
| Reference | 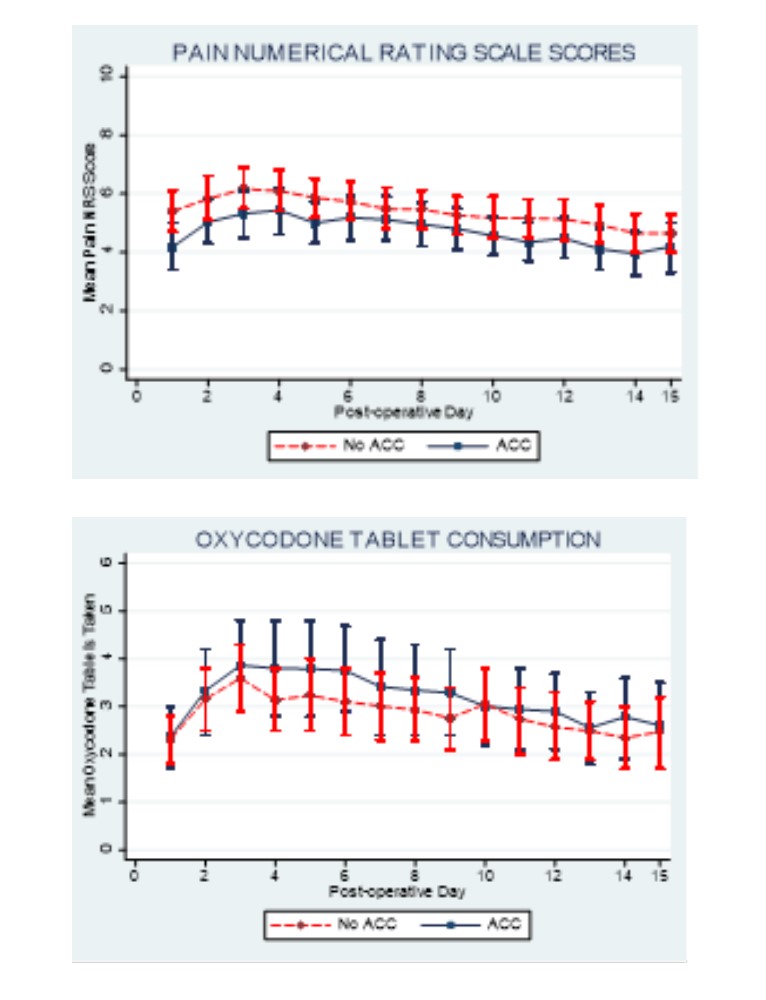 Manuscript Submitted |
| Authors | Jonathan E. Volk, MD MPH, Michael Silverberg, PhD MPH |
|---|---|
| Challenges | Many patients who are at risk for acquiring HIV would benefit from HIV preexposure prophylaxis (PrEP), but use remains limited and inequitable. Strategies to improve PrEP provision in primary care are urgently needed. |
| Existing Evidence | PrEP uptake remains limited and inequitable, despite having a Grade A recommendation from USPSTF; in 2021 PrEP was prescribed to only 30% of those likely to benefit. Flagging the 2% of the general patient population with the highest HIV risk scores, our previously developed model prospectively identified 39% of new HIV diagnoses (46% among males), substantially outperforming CDC criteria for PrEP use, particularly among Black patients, a population with high HIV incidence and low PrEP uptake. |
| Target Population | Non-HIV infected adult patients at KP San Francisco not previously prescribed HIV PrEP who have an estimated 3-year HIV incidence of ≥0.2% based on our EHR HIV prediction model. |
| Intervention or Exposure | Primary care providers at KP San Francisco, randomized to usual care or intervention (alerted via EHR-based staff messages prior to upcoming in-person or virtual visits and prompted to discuss HIV prevention and PrEP). |
| Outcomes/Key Findings |
A low-intensity EHR-based intervention guided by an HIV prediction model:
|
| Resulting Action/Change | The prediction score was integrated into the EHR and can be leveraged in the future, for patient outreach (e.g. outreach for e-visits, including the sexual health e-visits), to pharmacist co-management, and to enable providers to refer to PrEP with fewer barriers (e.g. best practice alert that emails patients links to PrEP e-visit). The risk score incorporated real-time patient data and facilitated provider notifications within routine workflows, informing future best practice alerts and other interventions to increase PrEP uptake. |
| Additional Recommendations | These results support evaluating targeted applications of this risk tool and integrating with newly developed virtual tools such as e-visits for STI testing and PrEP and exploration of other methods for providers who do not routinely provide HIV care (and their patients). |
| Implementation Tools | HIV risk calculator integrated into the EHR. |
| Implementation and Follow-up Measures |
Initiation of PrEP care defined as PrEP discussions, referrals, or prescription fills. |
| Reference | 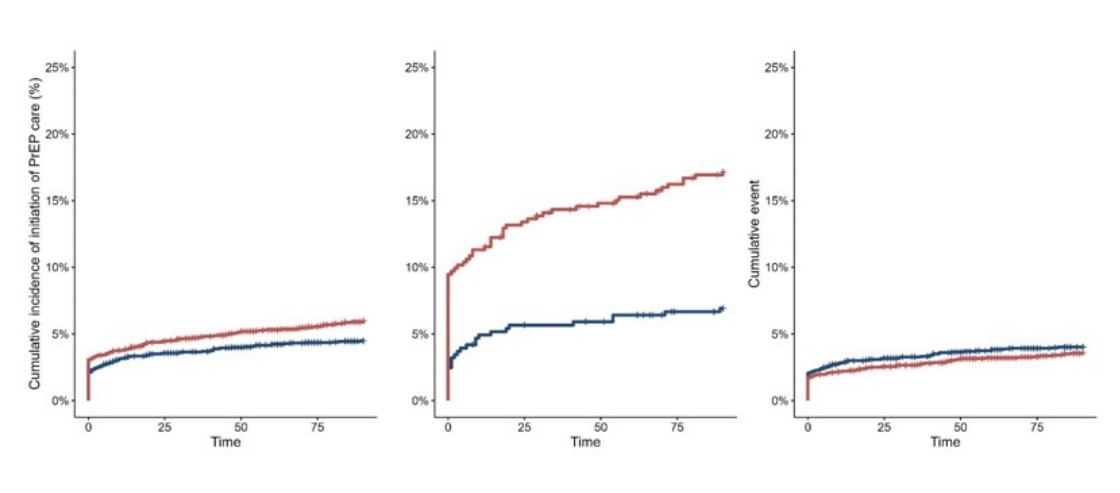 Manuscript Submitted |
| Authors | Alan Go, MD, Amir Axelrod, MD, Andrew Ambrosy, MD; Jitesh Vasadia, MD |
|---|---|
| Challenges | It is unknown whether novel, new, remote monitoring methods utilizing a comprehensive heart failure disease management program that includes telemonitoring and patient education might influence both health care utilization (such as emergency department care and hospitalization) and mortality |
| Existing Evidence | Four KPNC facilities (North Valley, South Sacramento, Santa Rosa and Napa-Solano) have used telemonitoring to follow and treat selected high-risk patients after a clinical encounter for worsening heart failure (HF). The benefit of telemonitoring from randomized trials is unclear, some reported potential clinical and resource utilization benefits, but most had small sample sizes (<900 patients) and were heterogenous in the type of telemonitoring. |
| Target Population | Eligible adults with heart failure at Roseville, Sacramento, South Sacramento, Santa Rosa, and Napa-Solano facilities between 2015-2019. |
| Intervention or Exposure | Use of a natural experiment within KPNC, with some patients receiving remote home-based telemonitoring using the Residio LifeStream system. Patients with & without telemonitoring were matched on age, sex, race/ethnicity, service area, left-ventricular ejection fraction, HF duration, and a high-dimensional ropensity score. |
| Outcomes/Key Findings | Adults with HF who received telemonitoring had more frequent medication adjustments but comparable rates of hospitalizations and emergency department visits for worsening HF and all-cause mortality than controls who did not receive telemonitoring |
| Resulting Action/Change | These results do not definitively recommend widespread adoption of telemonitoring for patients with heart failure, given these findings and uncertain benefit in randomized trials. |
| Additional Recommendations | An adequately powered randomized controlled trial may be necessary to establish confidence in benefits of telemonitoring for heart failure, overall or in targeted subgroups. These results reinforce the need for evaluating new devices and methods prior to widespread implementation. |
| Implementation Tools | None |
| Implementation and Follow-up Measures |
Proportions of patient using telemonitoring, emergency department utilization, hospitalization rates, and mortality. |
| Reference |  https://pubmed.ncbi.nlm.nih.gov/37220825/ |
| Authors | Joseph Presti, Jr., MD, Stacey Alexeeff, PhD, Brandon Horton, MPH, Stephanie Prausnitz, MS, Andrew L. Avins, MD, MPH, |
|---|---|
| Challenges | Currently only about 25% of men with mild PSA elevations have a prostate cancer that warrants treatment. Better risk assessment is needed. |
| Existing Evidence | No prospective evaluation of a prostate cancer risk calculator has been performed in men with mild PSA elevations. |
| Target Population | Men without prior biopsies who have mild PSA elevations (<10 ng/ml) |
| Intervention or Exposure | Use of the validated KP Prostate Cancer Risk Calculator 2.0 in counselling for possible biopsy |
| Outcomes/Key Findings |
Calculator usage led to a biopsy population enriched in high-grade cancer and fewer negative biopsies compared to historical controls and use for informed decision-making regarding prostate biopsy was accepted by patients and physicians.
|
| Resulting Action/Change | KP Prostate Cancer Risk Calculator can be considered for incorporation into HealthConnect for regular use in supporting clinicians and patients in shared decision making for prostate biopsies. |
| Additional Recommendations | The KP Prostate Cancer Risk Calculator is currently being built into HealthConnect. We have initiated work with Garfield funding to further study our calculator in KPSC and to refine it using some novel serum markers that are not currently available in KPNC but are being used in KPSC. |
| Implementation Tools | The risk calculator is available for next-step evaluation and use in different settings. |
| Implementation and Follow-up Measures |
Uptake of calculator, percentage accepting biopsy, biopsy outcomes. |
| Reference | 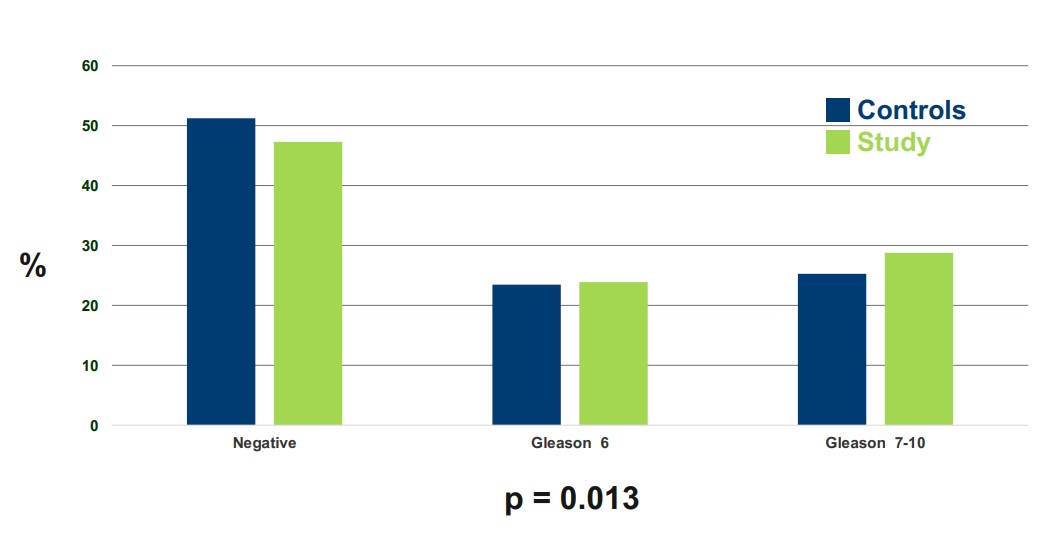 Presented at the Western Section American Urological Association Meeting, October 3, 2023 |
| Authors | Varun Saxena, MD MAS; Liyan Liu, MSc; Nizar Mukhtar, MD; Sreepriya Balasubramanian, MD MPH; Brock MacDonald, MD; Suk Seo, MD; Joanna Ready, MD; Julie Schmittdiel, PhD, MA |
|---|---|
| Challenges | Hepatocellular carcinoma (HCC) incidence has been the most rapidly increasing cancer for four decades. Little data exist for identifying high risk populations for recommended HCC screening, despite large at-risk KPNC patient populations with non-alcoholic fatty liver disease (NAFLD, estimated 200,000 members), treated hepatitis C (~13,000), and hepatitis B (HBV) (19,000 members). |
| Existing Evidence | For chronic hepatitis B and treated hepatitis C, there have been a few non-US cohort studies of uncertain generalizability risk-stratifying patients HCC risk. The population of people with fatty liver disease is even larger. |
| Target Population | Cohorts of adults diagnosed between 2006-2018 with NAFLD, treated HCV after cure, or HBV were evaluated. |
| Intervention or Exposure | For each cohort, we evaluated the performance characteristics of externally derived risk scores for HCC (for HBV and treated hepatitis C); derived new KPNC risk scores for all cohorts; and then compared the performance of internal vs. external approaches (as applicable). |
| Outcomes/Key Findings | KP derived risk scores performed better than externally derived risk scores to stratify patients into low, medium, and high-risk groups, to accurately identify those likely to benefit / not benefit from every-6-month surveillance ultrasounds & serum AFP. Among patients with NAFLD, the KPNC HCC risk score had an excellent ability (AUROC 0.88) to stratify patients into low-, medium-, and high-risk groups (Figure 1). Among patients treated for hepatitis C (N=12,758), the KPNC HCC risk score(AUROC .94) was superior to external scores such as aMAP (0.74, without cirrhosis, 0.63 with cirrhosis) or the Toronto risk score (0.75 without cirrhosis, 0.65 with cirrhosis) (Figure 2). Among patients with hepatitis B (N=30,287), the KPNC HCC risk score (AUROC 0.8) was superior to external scores (Figure 3) such as AGE-B (AUROC 0.82) and mPAGE-B (0.80). |
| Resulting Action/Change | KPNC derived HCC risk scores will be implemented to use deploy a risk-based approach to HCC screening among patients with treated NAFLD, treated HCV, and HBV. |
| Additional Recommendations | Working with KPNC IT to create real time HCC risk calculation within HealthConnect (or via toolbar), resultant HCC screening recommendations and population management |
| Implementation Tools | HCC risk stratification criteria that use electronic medical record variables. |
| Implementation and Follow-up Measures |
Use of risk stratification in patients with NAFLD, hepatitis C, and hepatitis B; cancer detection rates in patients by risk category |
| Reference | 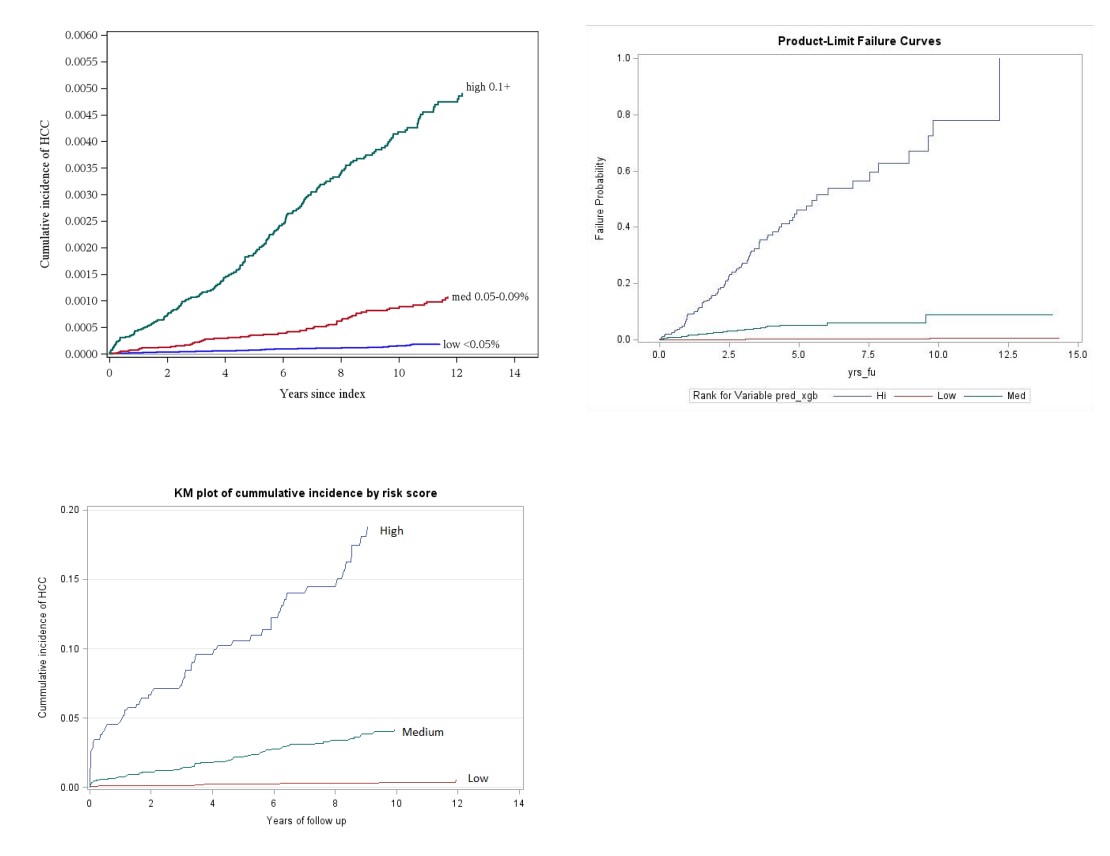 Manuscripts Underway |
| Authors | Vignesh A. Arasu, MD, PhD; Andrew L. Avins, MD, MPH; Laurel A. Habel, PhD; Jason D. Balkman, MD; Dorota J. Wisner, MD PhD; Dan Navarro, MD; Catherine Lee, PhD |
|---|---|
| Challenges | At KPNC, over 100 radiologists read screening mammograms and demonstrate a 12-fold difference in cancer detection rates, including some below common guideline thresholds. Efficient time-to-exam reading times are challenged by volumes and staffing shortages, potentially inducing diagnostic delays. |
| Existing Evidence | Retrospectively, we demonstrated that high AI risk scores can identify 25-50% of breast cancers missed at screening. Whether it can achieve similar results prospectively and also help with real-time exam prioritization for diagnosing cancers same-day is unknown. |
| Target Population | Women undergoing mammographic screening (predominately aged 40–75 years) |
| Intervention or Exposure | AI-based prioritization of mammography screening exam interpretation, including evaluation of 5 available commercial or open-source algorithms. |
| Outcomes/Key Findings |
A retrospective evaluation demonstrated that:
|
| Resulting Action/Change | Results led to region-wide trial to evaluate improvements in cancer detection, informed a KP-IT computer vision AI use case for national strategy, and proof-of-concept technology and workflows, and informed data & technology infrastructure needs for at scale AI actions. |
| Additional Recommendations | The results demonstrated the importance of prospectively evaluating technologies to inform adoption. Operational leaders can consider how results may inform TPMG AI strategy and development of proprietary workflows, as well as AI investments priorities. |
| Implementation Tools | Epic, Radiant |
| Implementation and Follow-up Measures |
Rate of rollout regionally, automated integration in workflow, cancer detection, time from mammogram to cancer diagnosis, cancer outcomes, diagnostic variability between radiologists after AI implementation |
| Reference | 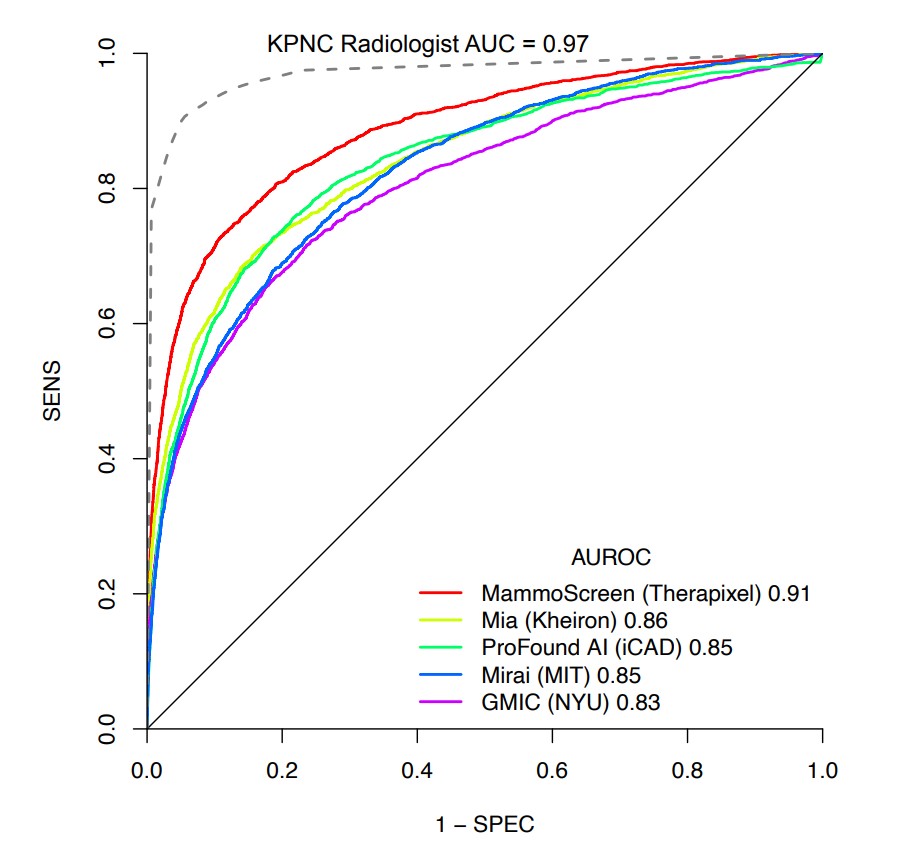 https://pubmed.ncbi.nlm.nih.gov/37278627/ |
Physician Researcher Program
| Authors | Kathryn K. Ridout, M.D., Ph.D., Chethana Eswarappa, M.D., Kelli Peterman, MS, Brooke Harris, Ph.D., Lyndsay Avalos, Dr.PH., Samuel J. Ridout, M.D., Ph.D. |
|---|---|
| Challenges | A large number of women with a history of depression take antidepressants, and many desire to stop medications during pregnancy. The impacts of continuing vs. stopping on the risk of post-partum depression (PPD) are unknown. |
| Existing Evidence | Postpartum depression (PPD) impacts 1 in 7 women in the United States, is a large risk factor for maternal suicide, and impacts maternal-infant bonding and infant cognitive-emotional development. The American College of Gynecologists and American Psychiatric Association recommends women with a history of poor response to psychotherapy alone, moderate to severe PPD, or recurrent depressive disorders outside of pregnancy have initiation or continuation of an antidepressant during pregnancy. |
| Target Population | Women ≥18 with a live birth delivery between 2010-2019, an antidepressant fill in the 6 month prior to last menstrual period, and a depression diagnosis in the prior year |
| Intervention or Exposure | Continuous antidepressant use during pregnancy. |
| Outcomes/Key Findings | Women with a history of depression who discontinued (vs. continued use) were more likely to develop postpartum depression overall, (adjusted relative risk (aRR): 1.14; 95%CI 1.06-1.22 and 1.14) and had a higher risk of severe post-partum depression (PHQ-9≥20 within one year after delivery; aRR=1.33; 95% CI 1.09-1.62). Similarly, women who intermittently used their antidepressants during pregnancy had a higher risk of PPD overall (aRR=1.14; 95%CI 1.05-1.24). Regardless of antidepressant status, women with at least mild (PHQ-9≥5) depressive symptoms during the first depression screening of pregnancy had higher risk of PPD overall (aRR=1.49-1.75), and severe PPD (aRR=2.13-2.52). The number needed to treat to see the benefit of continued antidepressant use during pregnancy to prevent PPD is 15. |
| Resulting Action/Change | Ability to inform patients and providers regarding antidepressant treatment in patients with pre-existing depression who are pregnant or planning pregnancy. |
| Additional Recommendations | Discussions with patients based on their history of depression and depression severity regarding the relative risks and benefits could help improve patient outcomes. |
| Implementation Tools | Risk estimates, diagnostic criteria for identifying patients at risk. |
| Implementation and Follow-up Measures |
Percentage of patients continuing antidepressants during pregnancy, post-partum depression diagnosis. |
| Reference | 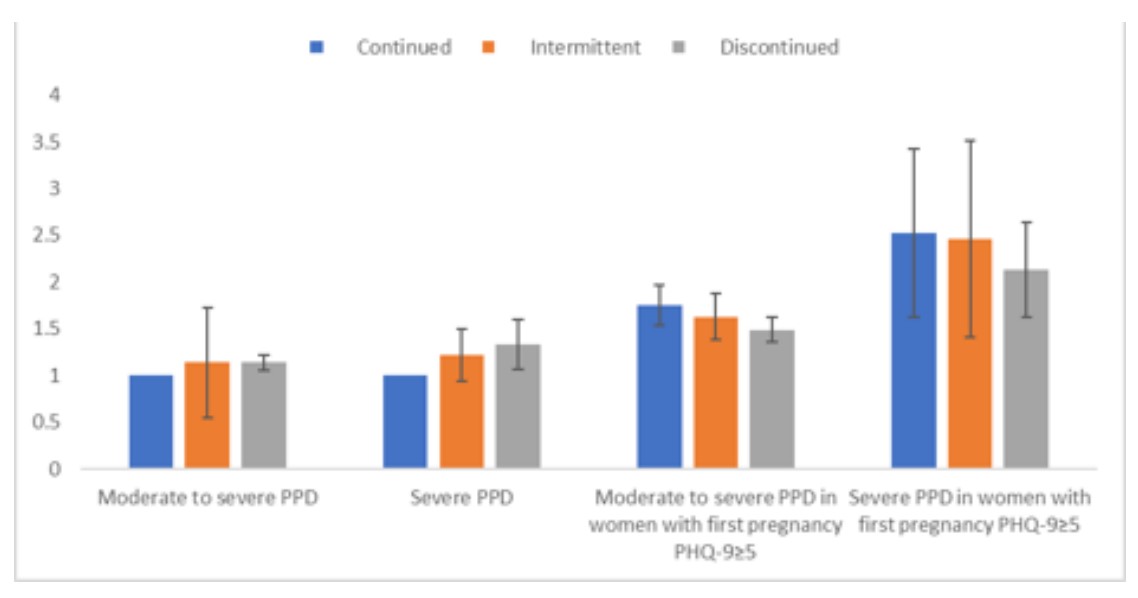 Manuscript Submitted |
Rapid Analytics Unit
| Authors | Kian C. Banks, MD; Jennifer R. Dusendang, MPH; Julie A. Schmittdiel, PhD, MA; Diana S. Hsu, MD; Simon K. Ashiku, MD; Ashish R. Patel, MD; Lori C. Sakoda, MPH, PhD; Jeffrey B. Velotta, MD |
|---|---|
| Challenges | National guidelines recommend large-scale lung cancer screening among at-risk patients and KPNC has instituted programs to fulfill this goal. However, the ideal time to surgery for early-stage lung cancer is unknown, including if currently recommended minimal diagnosis-to-surgery time recommendations accurately decrease the risk of stage progression. |
| Existing Evidence | The time between lung cancer diagnosis by radiologic imaging and subsequent surgical resection varies widely. This variation is influenced by the need for additional work-up, patient preference, and operative scheduling. Few studies have evaluated if there is an optimal minimum time to surgery, beyond which there is an increased risk of recurrence or stage progression to inform patients, providers, and large-scale lung cancer screening programs. |
| Target Population | Stage I or II lung cancer patients aged 18 to 85 years undergoing elective surgery who had CT or PET imaging within six months prior to surgery |
| Intervention or Exposure | Time from last CT or PET scan to surgery (TTS) |
| Outcomes/Key Findings |
Early-stage lung cancer patients with a time to surgery within 4 weeks experienced:
This suggests the maximum time to surgical resection after lung cancer diagnosis to optimize outcomes may be much shorter than previously recommended, though |
| Resulting Action/Change | The results inform clinicians, patients, and large-scale lung cancer screening programs (such as those at KPNC) regarding evidence-based care systems & targets for patients with early stage lung cancer. The findings will be shared with thoracic surgery; medical, surgical & radiation oncology; pulmonology; radiology and the regional screening program. The results may also modify current KP targets for surgery within two weeks, increasing flexibility for scheduling. |
| Additional Recommendations | These results inform potential changes to national society guidelines on optimal time to treatment for lung cancer patients. This analytic approach is applicable to other screening programs early-stage cancers, to guide health-system level program development and planning. |
| Implementation Tools | Data on time to surgery vs. outcomes, mechanisms for identifying at-risk patients |
| Implementation and Follow-up Measures |
Time to surgery, variation by medical center, cancer stage. |
| Reference | 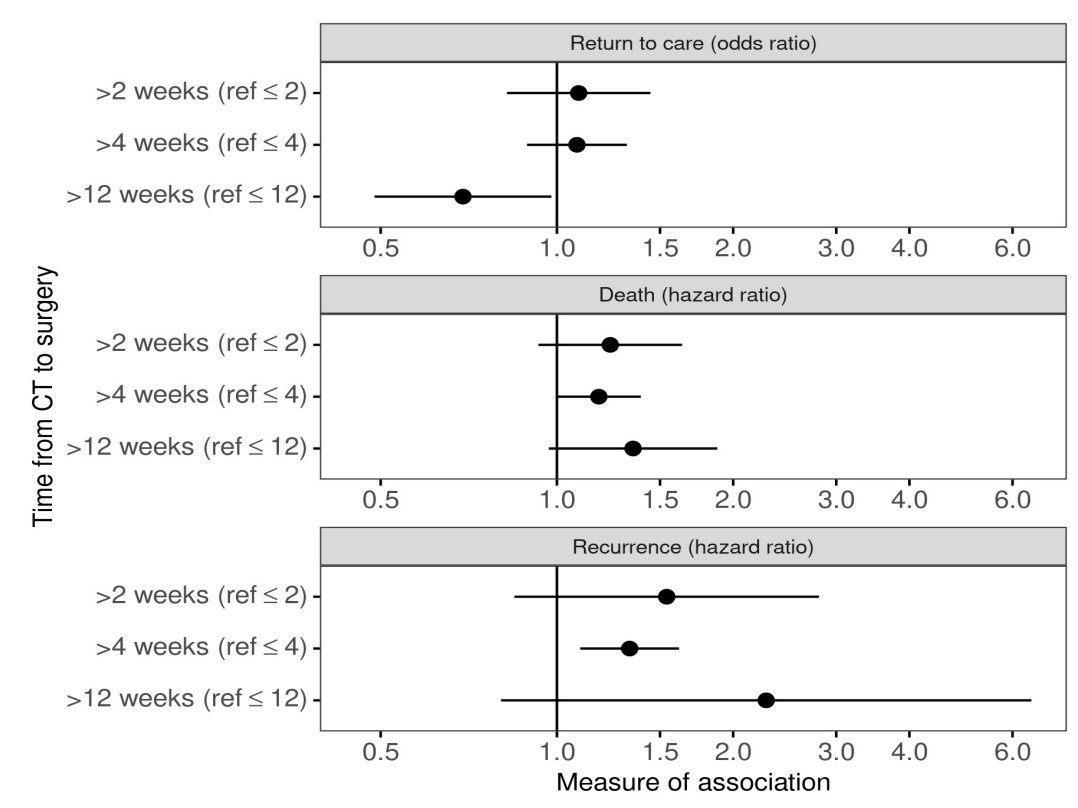 https://pubmed.ncbi.nlm.nih.gov/36695837/ |
| Authors | Lori C. Sakoda, PhD, MPH, Jie Zhang, PhD, Douglas A. Corley, MD, PhD, George Minowada, MD, Charles P. Quesenberry Jr, PhD, Sundeep M. Nayak, MD |
|---|---|
| Challenges | The implications of implementing the 2021 U.S. Preventive Services Task Force(USPSTF) lung cancer screening guidelines on the screening-eligible population and for decreasing demographic differences in screening are largely unknown. |
| Existing Evidence | In March 2021, the USPSTF revised their 2013 recommendations on lung cancer screening, expanding age eligibility to 55-80 years and smoking to ≥20 packyears, in part to increase eligibility for more Black/African American and women patients. The impacts on detection, screening volumes, and disparities are unclear. |
| Target Population | Population 1 – adults aged 50-80 years who ever smoked cigarettes, as of 06/30/2020; Population 2 -Adults diagnosed with incident primary lung cancer from 01/01/2014 to 12/31/2018. |
| Intervention or Exposure | Expanded screening criteria by age and fewer pack years smoked. |
| Outcomes/Key Findings |
Implementing new screening guidelines would:
Among ever smokers, changing eligibility criteria gains were similar across race categories (9.3%; 9.0%-9.6%); lower by Hispanic ethnicity (7.1%); and larger for men (9.9%) than women (7.9%). Among people diagnosed with a new lung cancer, new criteria eliminated prior screening eligibility differences between Black and White people (now 31.1% vs. 33.5%, respectively). Black people had the largest gains in eligibility (10.8%). |
| Resulting Action/Change | The new guidelines markedly expand the number of smokers eligible for screening. Healthcare systems will need to plan relevant resources to provide screening to the expanded pool of screening-eligible adults |
| Additional Recommendations | Additional strategies for early detection of lung cancer are needed for at-risk patients, as most who develop lung cancer are not recommended for screening |
| Implementation Tools | Number of people eligible for lung cancer screening in KPNC, for informing program resources & implementation |
| Implementation and Follow-up Measures |
Proportions of people identified as eligible for screening (smokers) from electronic records, proportions screened, differences by demographic groups. |
| Reference | 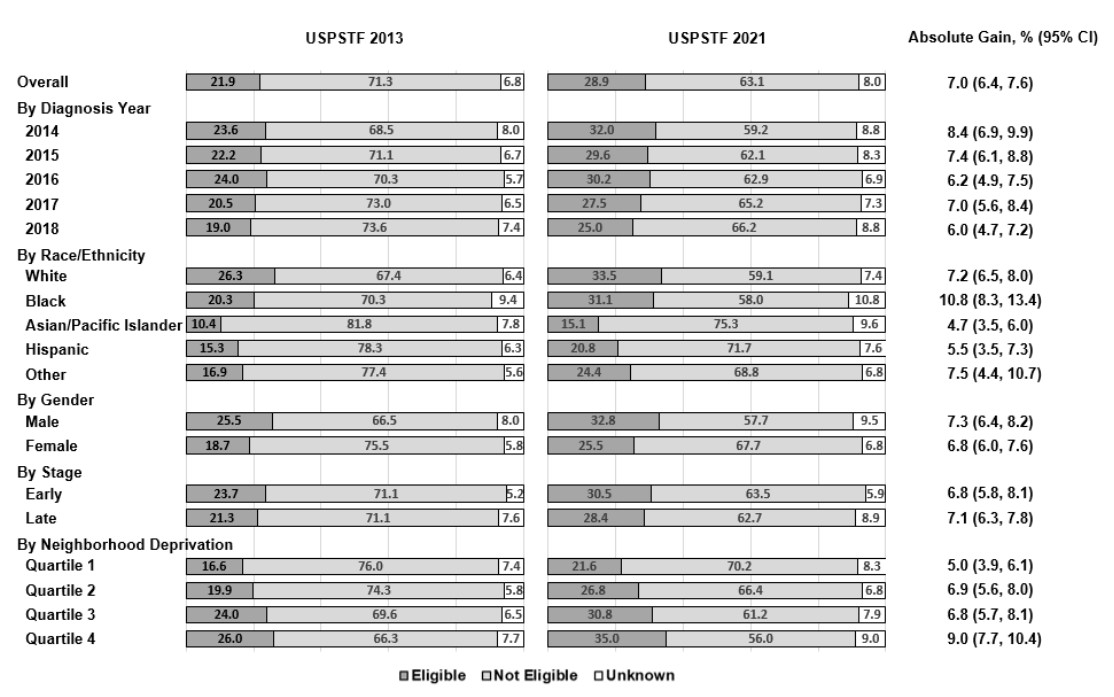 Manuscript Submitted |
Targeted Analysis Program
| Authors | Veronica Shim MD, Audrey Karlea MS LCGC, Leslie Manace Brenman MD MPhil, CK Chang, Jamila Gul BS, Elizabeth Hoodfar MS CGC, Tracy D Chan RN, Poline C Engeman NP, Vanessa M. Sheldon, RN, Deirdre M Thorne-Hadfield NP, Patience Odele MD, Brooke Vuong MD, Jennifer McEnvoy MD, Dinesh Kotak MD, Laurel Habel PhD. |
|---|---|
| Challenges | Genetic testing for many patients with cancers is becoming standard of care. The current clinical pathway of universal genetic counselor referral for testing is challenged by both patient attrition in the referral process and feasibility. In addition, current NCCN guidelines for testing aimed at younger age groups may not detect many older breast cancer patients with genetic changes. |
| Existing Evidence | “Mainstreaming” genetic testing within current clinical care pathways is a possible way to meet the increased need in genetic testing among breast cancer patients, while personalizing their care with providers who are already familiar to them. |
| Target Population | KPNC patients diagnosed with breast cancer |
| Intervention or Exposure | Breast care coordinators for genetic testing order and pretest counseling at 4 centers (Central Valley, EB, San Rafael, S. Sac) vs. standard pathways for genetic counsel referral at 11 other centers. Within the pilot program, onlypatients with abnormal genetic profiles (including variants of unknown significance) were referred to genetics. |
| Outcomes/Key Findings |
Offering genetic testing to all women under 65 with breast cancer through frontline breast cancer care coordinators vs. through genetic counselor referral:
A substantial portion of patients had variants of uncertain significance. (46.3% at pilot vs 54.2% at non-pilot sites) |
| Resulting Action/Change |
These findings recommend, among patients with breast cancer and potentially those with other cancers commonly associated with genetic syndromes:
|
| Additional Recommendations | Steps for broader “mainstreaming” of genetic testing for patients with breast cancer include: 1) coordination with breast care coordinators or clinicians at additional centers 2) training coordinators with protocols from the pilot centers 3) incorporation of care flows in the newHealthConnect® genomic module |
| Implementation Tools | Updating the HealthConnect® genetic module in 2023 by the national genomics team, to facilitate expansion of “mainstreaming” genetic testing |
| Implementation and Follow-up Measures |
Proportions of patients with breast cancer who complete genetic testing by age groups, proportions with positive tests, differences by demographics & medical center, and proportions who complete follow-up with genetic counseling for abnormal test results. |
| Reference | 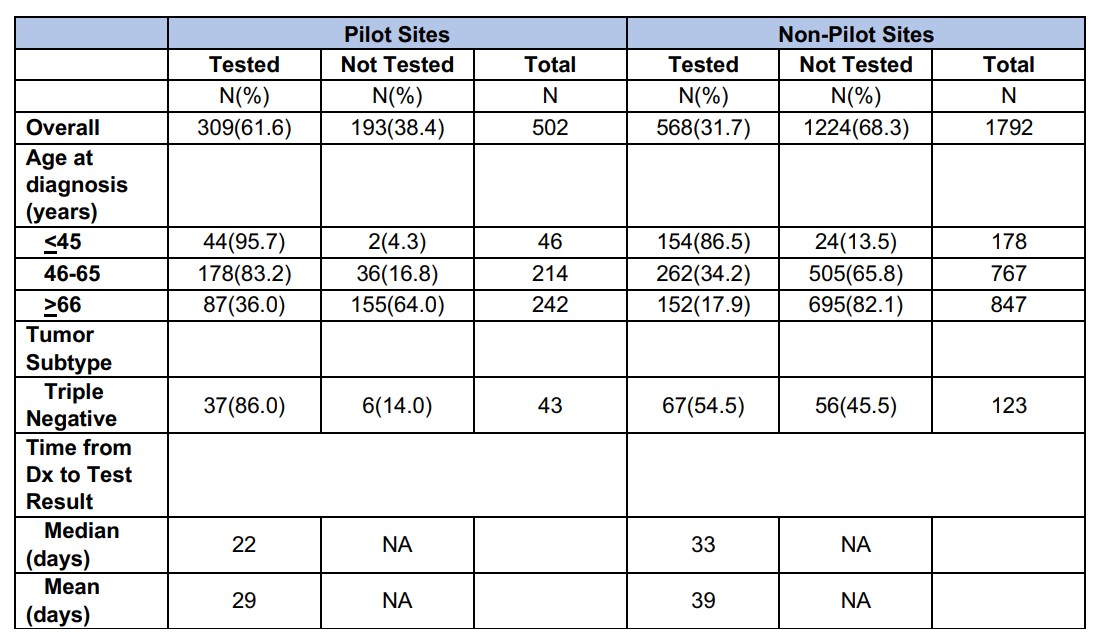 Manuscript Submitted |
DARE Supported Projects 2021-2023
| Anesthesiology | Brad Cohn, Vincent Liu | Evaluation of an Electronic Health Record-Based Risk Stratification Algorithm for Perioperative Medicine Triage |
| Anesthesiology, Surgery | Edward Yap, Mary Reed | Toward Reducing Surgical Complications After Urgent and Emergent Surgery |
| Cardiology | Drew Ambrosy | Defining the Role of ElectroNic HealTh Record-Based Alerts Worsening Heart Failure (IDENTIFY-WHF) Improves Care |
| Cardiology | Ed McNulty, Alan Go | Transcatheter aortic valve replacement (TAVR) – Personalizing risk for QOL, complications, total mortality, and utilization |
| Cardiology | Amir Axelrod, Andrew Ambrosy, Alan Go | No Differences in ED Visits, Hospitalizations, or Mortality Among Heart Failure Patients with Remote Telemonitoring |
| Cardiology, Health Care Delivery and Policy | Dustin Mark, Mary Reed | Validation of an Algorithm for ED Patients with Possible Acute Coronary Syndromes After Transition to a High-Sensitivity Troponin Assay |
| Cardiology, Population Care | Adam Rogers, Carlos Iribarren | Improving quality by TARGETing LDL using a systems-based approach to evaluate our current performance (TARGET-LDL) |
| COVID | Mary Reed, Dustin Ballard | Post-Acute Sequelae of SARS-Cov-2 Infection (PASC) in Adult KPNC Members |
| COVID | Tracy Lieu | Outreach to Enhance COVID-19 Vaccination Among Hesitant Elderly |
| COVID, Population Care | Gabriel Escobar, Laura Myers, Vincent Liu | Tools for Outpatient and Population Management of SARS-COV-2 Infections (TOPS2) |
| COVID, Ob/Gyn, Womens and Childrens Health | Mara Greenberg, Assiamira Ferrara | A Prenatal Care Strategy that Included Telehealth had Similar Outcomes as In-Person Visits |
| Emergency Medicine | David Vinson, Mary Reed | Reducing Variation in Hospitalization and Care in ED Patients with A-fib: A Stepped Wedge Cluster Randomized Trial |
| Endocrinology, Population Care | Lisa Gilliam, Richard Grant | Testing a new population management model for hypoglycemia prevention in high-risk KPNC members |
| Gastroenterology | T.R. Levin, Jeffrey Fox, Jeffrey Lee | De-implementation of Outdated Colonoscopy Surveillance Interval for Patients with Low-risk Adenomas (DESIRE) |
| Gastroenterology | Jeff Lee, Theodore Levin | Understanding the Difference of Risk of Advanced Colorectal Neoplasia in Patients with Non-advanced Adenomas (3-4 vs 1-2) |
| Gastroenterology | Varun Saxena, Julie Schmittdiel | Novel Risk Stratification Optimizes Hepatocellular Carcinoma Surveillance Protocols and Guidelines |
| Infectious Disease, Primary Care | Jonathan Volk, Michael Silverberg, | Electronically Identifying Patients at Elevated Risk of HIV Increased Pharmacologic HIV Pre-exposure Prophylaxis Use: A Clinical Trial |
| Mental and Behavioral Health | Honor Hsin, Esti Iturralde | Development of a scalable and adaptable clinical workflow for machine learning (ML)-based suicide prevention in mental health care |
| Mental and Behavioral Health | Kevin Li , Esti Iturralde | Evaluation of electroconvulsive therapy, transcranial magnetic stimulation, and intravenous ketamine for treatment-resistant depression |
| Mental and Behavioral Health | Kathryn Erickson-Ridout, Connie Weisner | Evaluation of the Achieving Depression and Anxiety Patient Centered Treatment (ADAPT PLUS) Program |
| Mental and Behavioral Health, Ob/Gyn | Kathryn Erickson-Ridout, Lyndsay Avalos | Evaluation of the EmbrACE Intervention for Adults with a History of Adverse Childhood Experiences |
| Nephrology | Sijie Zheng, Alan Go | Kidney Disease Population Care |
| Neurology | Mai Nguyen-Huynh, Jeff Klingman | Extending Intravenous Tenecteplase Beyond 4.5-hour Window for Patients with Acute Ischemic Stroke |
| Ob/Gyn | Joanna Stark, Lyndsay Avalos | Evaluate “Centering Pregnancy”, a group prenatal care program, impact on health outcomes and health care utilization. |
| Ob/Gyn, Womens and Childrens Health | Mara Greenberg, Monique Hedderson | Evaluating patient engagement in “KP Connected Pregnancy Care” and its association with utilization and perinatal outcomes |
| Oncology | Raymond Liu, Gabriel Escobar, Vincent Liu | Automatic risk stratification for hospital-acquired VTE to improve utilization of risk-appropriate pharmacological prophylaxis |
| Oncology | Charles Meltzer, Lori Sakoda | Evaluating outcomes and efficiency of consolidated multidisciplinary care for head and neck cancer |
| Oncology | Bethan Powell, Larry Kushi | Genetic testing of women with hereditary breast and ovarian cancer syndrome |
| Oncology | Jed Katzel, Stephen Van Den Eeden | Implementation of Patient Reported Outcomes in Head and Neck Cancer |
| Oncology | Stephen Van Den Eeden, | Physical Function in Pancreatic Cancer Patients |
| Oncology, Population Care, Urology | Joseph Presti, Andy Avins | Improving shared decision making for prostate cancer screening |
| Oncology, Surgery | Veronica Shim, Laurie Habel | Developing a TPMG Pathway for Selective Oncotype Testing in Early Breast Cancer |
| Optometry/Ophthalmology | Dariusz Tarasewicz, Oleg Sofrygin | Implementation of an evidence-based risk calculator for diabetic retinopathy screening and population management |
| Orthopedics | Adrian Hinman, Andy Avins | Adductor Canal Catheters not Superior to Conventional Therapy for Postoperative Pain Management After Total Knee Arthroplasty: A Trial |
| Pediatrics | Meghan Davignon, Lisa Croen | Evaluation of More Than Words Program at KPNC |
| Pediatrics | Josephine Lau, Stacy Sterling | Identifying Best Practices of Early Phase Pediatric Eating Disorder Care |
| Pediatrics | Lisa Chyi, Michael Kuzniewicz | Use of a modified Eat, Sleep, Console tool for management of Neonatal Abstinence Syndrome |
| Pediatrics | Michael Kuzniewicz, Dan Brugger | Predictive Analytics for Newborn Bilirubin Management |
| Pediatrics | Mustafa Bseikri, Elizabeth Feliciano | Pediatric Obstructive Sleep Apnea: Predictive Modeling to Streamline Care |
| Population Care | Lisa Gilliam, Andrew Karter | Comparative effectiveness of intermittently scanned continuous glucose monitoring vs. self-monitoring of blood glucose among insulin-treated type 2 diabetes patients |
| Population Care | Lisa Gilliam, Andrew Karter | Implementation of evidence-based risk stratifiaction tools for diabetic retinopathy screening and population management |
| Population Care, Mental and Behavioral Health | Lisa Fazzolari, Esti Iturralde | Population management for schizophrenia, schizoaffective disorder, and bipolar disorder utilizing trained psychiatric pharmacists |
| Primary Care | Maisha Draves, Lisa Herrinton | A Randomized, Multi-Drug De-Prescribing Intervention did not Change Medication Use or Geriatric-Syndrome Diagnoses. |
| Primary Care | Joan Lo, Kendal Hamann | Assessment of fracture prevention quality measures |
| Primary Care | Somalee Banerjee, Alyce Adams | Improving Outcomes and Care Experience among Dual Eligible Members: The Role of Health System Factors |
| Pulmonology, Thoracic Surgery | Eduardo Solbes, Laura Myers | Use and outcomes of intrapleural fibrinolytic therapy for complicated parapneumonic pleural effusion and empyema |
| Radiology | Vignesh Arasu, Laurel Habel | Prospective Mammography AI Evaluation Improved Cancer Detection and Time-to-Detection |
| Surgery | Amanda Graff-Baker, Marilyn Kwan | Lymphatic Microsurgical Preventative Healing Approach to Prevent Lymphedema in Patients Undergoing Axillary Lymph Node Dissection for BrCA |
| Urology | Joseph Presti, Andrew Avins | Novel KP Prostate Cancer Risk Calculator Leads to Better Selection of Men Needing a Biopsy in Those with Mild PSA Elevations |
| Anesthesiology | Edward Yap, Lisa Herrinton | Assessing variation in the incidence of myocardial injury after non-cardiac surgery (MINS) across medical centers and over time |
| Anesthesiology | Jonathan Khersonsky, Cynthia Campbell | Association of Nerve Blocks with Hospital Length of Stay for Surgical Abdominal Procedures |
| Cardiology | Kavin Desai, Lisa Herrinton | Accuracy of Prenatal Detection of Clinically Significant Congenital Heart Disease Among Still- and Live-Births |
| Cardiology | Richard Birnbaum, Andy Avins | Familial hypercholesterolemia II – manuscript |
| Cardiology | Richard Birnbaum, Andy Avins | Familial Hypercholesterolemia Implementation |
| Cardiology | Uma Vadlakonda, Mary Reed | Improved Outcomes with Home-Based Cardiac Rehabilitation-Experience from a Large Integrated Heathcare System |
| COVID, Mental and Behavioral Health | Kathryn Ridout, Esti Iturralde | Mental Health Service Demand in the face of COVID-19 |
| COVID, Physical and Rehabilitation Medicine | Joshua Rittenberg, Julie Schmittdiel | Association Between Injected Corticosteroids and Risk for Influenza and COVID-19 |
| Dermatology, Pharmacy | Veena Vanchinathan, Andy Avins | Optimizing Acne Care: What is the Impact of Isotretinoin? |
| Dermatology, COVID | Patrick McCleskey. Lisa Herrinton | Epidemiologic Analysis of Chilblains Eruptions at the time of COVID19 |
| Emergency Medicine | Mamata Kene, Mary Reed | Impact of Opioid Safety Initiative Education on Emergency Department Opioid Prescribing |
| Emergency Medicine | Dustin Mark, Mary Reed | Trends in the use of computed tomographic cerebral angiography for emergency department patients with headache |
| Emergency Medicine, COVID | Dale Cotton, Mary Reed | Characteristics of ED Patients Who Test Positive for SARS-CoV-2 in a Community Health Setting |
| Gastroenterology | Krisna Chai, Joanna Ready, Andy Avins | An Organized Hepatitis B Surveillance Program increases Patient Identification and Optimizes Management |
| Gastroenterology | Varuna Saxena, Julie Schmittdiel | Benefits of Hepatitis C Virus Cure |
| Gastroenterology | Krisna Chai, Joanna Ready, Andy Avins | Implementation success of integrated program on hepatitis B identification, surveillance, and treatment |
| Gastroenterology, COVID | Fernando Velayos, Julie Schmittdiel | COVID-19 Complications Are Not More Common Among Immunosuppressed Populations in KPNC |
| Gastroenterology, Oncology, Population Care | Sreepriya Balasubramanian, Julie Schmittdiel | Effect of Screening for Hepatocellular Carcinoma on cancer-related and all-cause mortality in patients with cirrhosis |
| Head and Neck, Radiology | Kevin Wang, Andy Avins | Improving Diagnostic Efficiency of Adult Neck Masses |
| Infectious Disease | Fernando Velayos, Julie Schmittdiel | Risk of COVID-19 pandemic on immunosuppressed populations |
| Infectious Disease, Hospital Medicine | Meredith Silverman, Cynthia Campbell | Vancomycin area under the curve-guided dosing and monitoring in the outpatient setting |
| Mental and Behavioral Health | Kathryn Ridout, Lyndsay Avalos | Continuation of Antidepressant Use During Pregnancy Lowers Risk of Postpartum Depression |
| Mental and Behavioral Health | Samuel Ridout, Cynthia Campbell | Integration of mobile health (mHealth) based interventions in mental health |
| Mental and Behavioral Health, Ob/Gyn | Carey Watson, Cynthia Campbell | The impact of ACEs and resilience on Obstetric health outcomes |
| Neurology | Josiah Ambrose, Cynthia Campbell | Surgical Epilepsy Center Referral Time Within an Integrated Health Care Network |
| Neurology, Population Care | Jeff Klingman, Abby Eaton | Stroke EXPRESS: Transition to TNKase |
| Ob/Gyn, COVID | Eve Zaritsky, Andy Avins | The Impact of California Shelter-In-Place on Incidence of Gynecologic Emergencies in a Community-Based Population |
| Ob/Gyn, Primary Care | Mehreen Khan, Mary Reed | Remote Patient Monitoring Assessment |
| Oncology | Robert Li, Lisa Herrinton | Changes in utilization, staging, and treatment after implementation of regionalized care for upper gastrointestinal cancer |
| Oncology | Tom Urbania, Lisa Herrinton | Evaluation of structured reporting of lung nodules detected on chest CT |
| Oncology, COVID | Ashok Pai, Gwendolyn Ho, Julie Schmittdiel | The impact of the use of anticoagulants and antiplatelets on the risk of hospitalization and mortality in patients with COVID-19 |
| Oncology, Surgery | Kourosh Kojouri, Lisa Herrinton | PAN 3: Efficacy and Value |
| Oncology, Population Care | Raymond Liu, Julie Schmittdiel | Cancer outcomes with KPNC vs. national community averages: an overview study |
| Oncology, Radiology | Lori Sakoda, Sundeep Nayak | Implementing Updated Lung Cancer Screening Guidelines Would Likely Decrease Demographic Disparities Found in Existing Practices |
| Optometry/Ophthalmology | Naveen Chandra, Marilyn Kwan | Dropless Cataract Surgery |
| Optometry/Ophthalmology | I-Hui (Elaine) Wu, Mary Reed | Outcomes of telemedicine in Ophthalmology |
| Optometry/Ophthalmology | Catherine J. Choi, Lisa Herrinton | Neurotrophic keratopathy: Incidence, presentation, utilization, and outcomes before adoption of corneal neurotization |
| Orthopedics | John Cox, Andy Avins | Perioperative VTE risk in total joint patients who had COVID-19 |
| Pediatrics | Josephine Lau, Julie Schmittdiel | Delivery of Inpatient Pediatric Eating Disorder Care in a Large Integrated Health Care Delivery System |
| Pediatrics, Hospital Medicine | Kelsey Childress, Marilyn Kwan | Reducing Blood Culture Contamination and Subsequent Healthcare Reutilization in Pediatrics |
| Pediatrics, Surgery | Albert Chong, Lisa Herrinton | Implementation of Evidence-Based Surgery for Pediatric Hernia Repair |
| Physical and Rehabilitation Medicine | Mamie Air, Julie Schmittdiel | Yearly corticosteroid burden of patients receiving spinal corticosteroid injections |
| Plastic Surgery | Todd Theman, Julie Schmittdiel | Safety and Efficacy of Corticosteroid Choice in Trigger Finger Injection |
| Primary Care | Kevin Wang, Janet Lai, Andy Avins | Improving Human Papilloma Virus Immunization Rates in Kaiser Permanente Northern California |
| Pulmonology, COVID | Nareg Roubinian, Julie Schmittdiel | Incidence of outpatient thromboembolism in patients with SARS-CoV-2 infections |
| Surgery | Reza Rahbari, Lisa Herrinton | Implementation and Outcomes Following Regionalization of Adrenal Surgery |
| Surgery | Simon Ashiku, Andy Avins | Minimally invasive esophagectomy |
| Surgery, COVID | Gillian Kuehner , Mary Reed | How COVID Changed Our Practice: Telehealth in TPMG Surgical Cancer Care |
| Thoracic Surgery | Jeffrey Velotta, Lisa Herrinton | Body weight changes with gastrostomy or jejunostomy feeding tube, esophageal stent, or no intervention in esophageal cancer patients starting chemotherapy and chemoradiation |
| Thoracic Surgery | Jeffrey Velotta, Julie Schmittdiel | Identifying Surgical Timing to Optimize Outcomes for Early-Stage Lung Cancer Surgery |
| Vascular Surgery | Nayan Sivamurthy, Julie Schmittdiel | Assessing the Impact of a Mobile Application Based Supervised Exercise Therapy (SET) Program for Peripheral Arterial Disease (PAD) |
| Cardiology | Matthew Solomon, Alan Go | Optimizing Management of Valvular Heart Disease |
| Emergency Medicine | David Vinson, Mary Reed | Improving management of ED patients with undifferentiated syncope; prospective validation of the Canadian Syncope Risk Score |
| Emergency Medicine | Dana Sax, Mary Reed | Improving Risk Stratification of ED Patients with Acute HF using a Machine-learning Platform for Personalized, Accurate, Real-time Risk Prediction |
| Gastroenterology | Dan Li | Improving health outcomes and reducing healthcare costs in individuals with Helicobacter pylori infection |
| Gastroenterology | T.R. Levin, Jeffrey Lee, Vincent Liu | PREDICT PCCC: PREDICTing Post Colonoscopy Colorectal Cancer |
| Infectious Disease, COVID | Jacek Skarbinski | Immunity and patterns of disease exposure for COVID-19 across Kaiser Permanente Northern California |
| Mental and Behavioral Health | Matthew Hirschtritt, Stacy Sterling | A mixed-methods, longitudinal analysis of a novel telepsychiatry assessment, brief treatment, and referral clinic model |
| Mental and Behavioral Health | Kathryn Erickson-Ridout, Constance Weisner, Esti Iturralde | Evaluation of the ADAPT PLUS program as a model for care delivery to outpatients with depression and anxiety |
| Neurology | Mai Nguyen-Huynh, Alan Go, Bruce Ovbiagele | Extended window for thrombectomy: Have we extended our resources appropriately and effectively? |
| Ob/Gyn, Population Care, Infectious Disease, | Betty Suh-Burgmann | HPV self-collection |
| Radiology | Vignesh Arasu, Laurel Habel | Improved selection of BRCA-negative high-risk women for breast MRI screening through validation of IBIS risk model variants |
| Urology | Joseph Presti, Andy Avins | Refining Shared Decision Making in Prostate Cancer Screening and Detection |
| Vascular Surgery | Robert Chang, Andy Avins | Optimizing Abdominal Aortic Aneurysm Surveillance and Intervention to Prevent Rupture |
| Allergy/Immunology, COVID | Lindsay Finkas, Carlos Iribarren | Retrospective analysis of incidence and health outcomes of asthma patients with COVID-19 within a large multi-site healthcare system |
| Anesthesiology, COVID, Hospital Medicine | Laura Myers, Kevin Ng | Trend in treatment location of patients with Covid-19 infection in an integrated health system |
| Emergency Medicine, Surgery, Thoracic Surgery | Jeffery Velotta, Vinnie Liu | Comparion of outcomes of video assisted thoracic surgery (VATS) versus robot assisted thoracic surgery (RATS) for lobectomy |
| Endocrinology, Ob/Gyn, Womens and Childrens Health | Mara Greenberg, Monique Hedderson | Remote Glucose Monitoring in Pregnancies with Gestational Diabetes: Assessing Uptake and Outcomes |
| General Surgery, Genetics/Genomics, Oncology | Veronica Shim, Laurel Habel | Streamlined, Risk Based Multi-Gene Testing of Women with Breast Cancer in KPNC |
| Hospital Medicine | Michael Yoo, Vinnie Liu | Evaluation of physical function measure by the PF-5 in Kaiser Permanente Northern California |
| Mental and Behavioral Health | Kevin Li, Esti Iturralde | Electroconvulsive therapy, anesthetic choice, and real-world patient outcomes |
| Primary Care | Rajiv Misquitta, Issac Ergas | Bodyweight, cholesterol, and glycemic control among patients with CHD and/or type 2 diabetes: a diet and lifestyle intervention program |
| Radiology | Sundeep Nayak, Lori Sakoda | Assessing eligibility, participation, and initial outcomes in lung cancer screening |
| Urology | Mark Gasparini, Stephen Van Den Eeden | Significance of borderline high and high serum calcium levels in high risk kidney stone patients in a community practice |